Scientists create ‘biological pacemaker’ inside off-tempo hearts
Researchers at Cedars-Sinai Heart Institute use gene therapy to create biological pacemaker cells in the hearts of living pigs. The findings could point the way to therapies that could replace surgically implanted electronic devices.
Pacemakers have long been a life-saving device for people whose hearts don’t keep the right beat – but they can sometimes come with complications. Now, a team of researchers at the Cedars-Sinai Heart Institute in Los Angeles have managed to transform regular heart cells in pigs into pacemaker cells – cells that naturally keep the heart’s rhythm in step.
The experiments described in the journal Science Translational Medicine mark the first study of this gene therapy in a large animal – one on par with human scale. The research could help lead to therapies for people who have to have their electronic pacemakers temporarily removed because of infection – and could one day remove the need for surgically implanted pacemaker devices altogether.
The heart beats to the sound of its own drum. It relies on a smaller number of specialized ‘pacemaker’ cells in a tiny region of the heart called the sinoatrial node – they are the metronome for the heart. But sometimes the heart can’t hear its own timekeeper. It beats too slowly or irregularly – and this can lead to dangerous consequences, from fatigue to circulatory collapse.
The researchers found a way around this problem: Create new pacemaker cells in a different part of the heart.
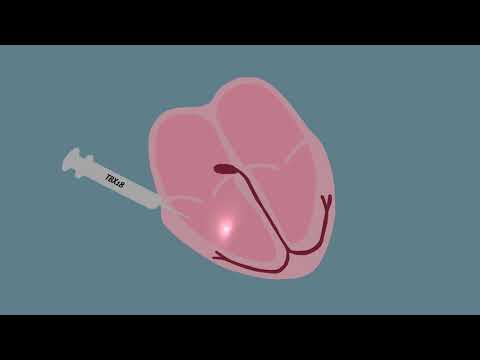
The therapy centers around a gene called TBX18, which is known as a transcription factor – a type of gene that creates a protein that turns other genes on and off. The researchers knew that the TBX18 gene was temporarily turned on in the area of the sinoatrial node as an embryo develops, and then it shuts off.
“That gave us a clue that maybe TBX18 is important in shaping the biological, the endogenous pacemaker to begin with,” said team leader Dr. Eduardo Marbán, director of the Cedars-Sinai Heart Institute.
The researchers loaded the gene into a virus and injected it into normal heart cells in pigs that suffered from complete heart block, which is when scarring keeps the electrical signals from the pacemaker cells in the sinoatrial node from getting through to the rest of the heart. They injected them into a different area of the heart, outside the sinoatrial node. In a matter of days, the injected pigs’ hearts were beating faster without the help of a pacemaker – and without any obvious adverse side effects.
“Nothing fancy needs to be done to see if the treatment is working,” said study co-author Dr. Eugenio Cingolani. And though the study only lasted 14 days, it could point the way to longer-lasting – even permanent – biological pacemakers. If all goes well, clinical trials on humans could start in three years. One day, he said, patients could potentially “be cured of the slow heart rate forever.”
In the meantime, there are a number of more specialized applications for such a gene therapy. For some fetuses with congenital heart block – many of whom develop severe heart problems that end in stillbirth – a biological pacemaker could be a lifesaver, since an electronic one can’t be surgically implanted in the womb.
Roughly 300,000 patients in the U.S. get a pacemaker every year, and about 2% of them develop infections, Marbán said. A significant portion of those people need to have their implants taken out and fixed or changed while the body heals, which could take several. The biological pacemaker could be one way to keep their hearts beating properly in the meantime.
“The lack of clinically adverse effects in the study is encouraging,” Eric Olson and Dr. Nikhil Munshi, researchers at UT Southwestern Medical Center in Dallas who were not involved in the paper, wrote in a commentary in the journal Science. But they added that after a two-week study, little is known about the long-term consequences, pointing out that the virus also ended up causing low-low level infections in the lung and spleen.
Still, they wrote, the findings “represent a critical step toward potentially filling an important clinical niche and provide an encouraging indication that a biological pacemaker might eventually be ready for human translation.”
Follow @aminawrite for more science news on matters of the heart.